Abstract
Objectives: To identify the psychosocial factors of periodontal disease and their impact on the quality of life of patients.
Methods: A mixed quantitative and qualitative study was conducted at the School of Dentistry, UdelaR. The instruments used were a semi-structured interview based on grounded theory and the application of the OHIP-14 (Oral Health Impact Profile) questionnaire that measures the degree of impairment of quality of life (Locker’s theoretical model).
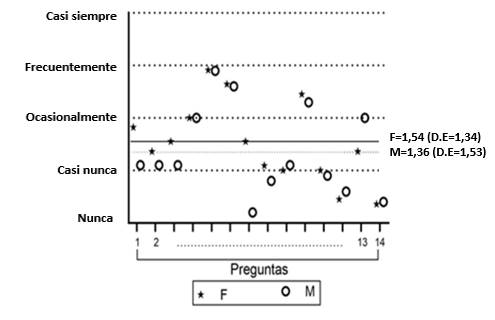
Results: This population’s psychosocial factors are identified, as well as the emotional and social effects of periodontal disease diagnosis. The results show a 1.46 impact on people’s quality of life on a scale of 0-4, where 4 is the maximum impact. Women showed a higher level of impairment in quality of life (1.54) than men (1.36). The higher the educational level, the more the quality of life is affected.
Conclusions: The limitations of the biomedical approach to dental patient care and the need for a comprehensive approach in periodontal disease patients are clear. Dental professionals need a biopsychosocial care approach given the complexity of periodontal disease.
References
2. Pihlstrom BL, Michalowicz BS, Johnson NW. Periodontal diseases. The Lancet. 2005; 366(9499): 1809-20.
3. Lorenzo S, Alvarez R, Andrade E, Piccardo V, Francia A, Massa F, Correa MB, Peres MA. Periodontal conditions and associated factors among adults and the elderly: findings from the first National Oral Health Survey in Uruguay. Cad Saúde Pública. 2015; 31(11): 2425 36.
4. Graves D, Zhenjiang D, Yingming Y. The impact of diabetes on periodontal diseases. Periodontology 2000 2020; 82: 214–224.
5. Carrizales E, Ordaz A, Vera R, Flores R. Periodontal disease, systemic inflammation and the risk of cardiovascular disease. Heart Lung Circ. 2018 Nov;27(11):1327-1334
6. Martinez M 1, Silvestre J, Silvestre F. Association between obesity and periodontal disease. A systematic review of epidemiological studies and controlled clinical trials. Med Oral Patol Oral Cir Bucal. 2017; 22 (6): 708-15.
7. Wong L, Yap A, Allen P. Periodontal disease and quality of life: Umbrella review of systematic reviews. J. Periodont. Res.. 2020;00:1–17 10.1111/jre.12805
8. Kaplan BH, Cassel JC, Gore S. Social support and health. Med Care. 1997; 15 :47-58
9. Elter J, White A, Gaynes B, Bader J. Relationship of Clinical Depression to Periodontal Treatment Outcome. J Periodontol. 2002; 73: 441-449.
10. Warren KR, Postolache TT, Groer ME, Pinjari O, Kelly DL, Reynolds MA. Role of chronic stress and depression in periodontal diseases. Periodontol 2000. 2014; 64(1): 127-38.
11. Dapueto J, Varela B. Modelos y praxis psicológicos en la medicina. Montevideo: Psicología Médica, 2016
12. Tizón García JL. Componentes psicológicos de la práctica médica, una perspectiva desde la atención primaria. Barcelona: Doyma, 1988. 272p
13. Martín Alfonso L. Aplicaciones de la psicología en el proceso salud enfermedad. Rev Cub Salud Pública 2003; 29(3): 275–281.
14. Peruzzo DC, Benatti BB, Ambrosano GM, Nogueira-Filho GR, Sallum EA, Casati MZ, Nociti FH Jr. A systematic review of stress and psychological factors as possible risk factors for periodontal disease. J Periodontol 2007; 78: 1491-1504
15. Moss ME. Exploratory case-control analysis of psychosocial factors and adult periodontitis. J Periodontol. 1996; 67(10): 1060-9.
16. Goffman E. Estigma. La identidad deteriorada. Buenos Aires: Amorrortu, 1963
17. Abrahamsson K, Wennströma J, Hallbergc U. Patients’ Views on Periodontal Disease; Attitudes to Oral Health and Expectancy of Periodontal Treatment: A Qualitative Interview Study. Oral Health Prev Dent 2008; 6: 209–216.
18. Locker D, Allen F. What do measures of “oral health-related quality of life”measure? Community Dent Oral Epidemiol. 2007 Dec;35(6):401-11
19. Meeberg GA. Quality of life: A concept analysis. J Adv Nurs 1993; 18: 32- 38.
20. García-Viniegras C, González Benítez I. La categoría bienestar psicológico. Su relación con otras categorías sociales. Rev Cubana Med Gen Integr 2000;16(6):586-92
21. Walker A. Understanding Quality Of Life in Old Age. Berkshire England: Open University Press, 2005.
22. Declaración de Helsinki de la Asociación Médica Mundial. Gac Med Mex 2001; 137(4): 387-390
23. Montero J, Bravo M, Albaladejo A, Hernández L, Rosel E. Validation the oral health impact profile (OHIP-14sp) for adults in Spain. Med.Oral Patol Oral Cir Bucal 2009;14(1): 44-50
24. Decker A, Askar H, Tattan M, Taichman R, Wang HL. The assessment of stress, depression, and inflammation as a collective risk factor for periodontal diseases: a systematic review. Clin Oral Investing 2020; 24(1): 1-12.
25. Lacopino A. Relationship between stress, depression and periodontal disease J Can Dent Assoc 2009 Jun;75(5):329-30
26. Morales Calatayud F. Psicología de la salud. Realizaciones e interrogantes tras cuatro décadas de desarrollo. Rev. Latinoamericana de Ciencia Psicológica. 2012; 4(2): 98-104.
27. Strauss A, Corbin J. Grounded theory methodology: An overview. En: N. K. Denzin & Y. S. Lincoln (Eds.), Handbook of qualitative research 1994; p. 273–285.
28. Slade GD. Derivation and validation of a short-fortn oral health impact profile. Community Dent Oral Epidemiol 1997; 25(4):284-90
29. Slade GD. Measuring Oral Health and Quality of Life.: Chapel Hill: University of North Carolina. Department of Dental Ecology School of Dentistry. 1997 Disponible en: https://www.adelaide.edu.au/arcpoh/downloads/publications/reports/miscellaneous/measuring-oral-health-and-quality-of-life.pdf
30. Arrivillaga M, Salazar I, Gómez I. Prácticas, creencias y factores del contexto relacionados con estilos de vida de jóvenes y adultos. Pontificia Universidad Javeriana. Psicología Conductual. 2005;13(1): 19-36
31. Cavallo F, Zambon A, Borraccino A, Raven-Sieberer U, Torsheim T, Lemma P. HBSC Positive Health Group. Girls growing through adolescence have a higher risk of poor health. Qual Life Res 2006;15: 1577-85.
32. Serra-Sutton V, Rajmil L, Aymerich M. Estrada MD. Desigualtats de genero en la percepció de la salut durant l´adolescencia. Annals de Medicina. 2004; 87: 25-9.
33. Muñiz E. Pensar el cuerpo de las mujeres: cuerpo, belleza y feminidad. Una necesaria miranda feminista. Soc. Estado 2014; 29(2). Disponible en: https://doi.org/10.1590/S0102-69922014000200006
34. Solano F, Ortiz V. La estetización del mercado laboral: modelos estéticos demandados por el trabajo en las sociedades contemporáneas. Antropol. Sociol. 2015; 17(2): 15-36
35. León S, Bravo-Cavicchioli D, Correa-Beltrán G, Giacaman R. Validation of the spanish version of the Oral Health Impact Profile (OHIP-14Sp) in elderly Chileans. BMC Oral Health. 2014; 14:95
36. Slade GD, Sanders AE. The paradox of better subjective oral health in older age. J Dent Res 2011; 90 (11): 1279-1285
37. Oppermann R, Hass A, Kuchenbecker C, Susin C. Epidemiology of periodontal diseases in adults from Latin America. Perodontol.2000 2015; 67(1):13-33.