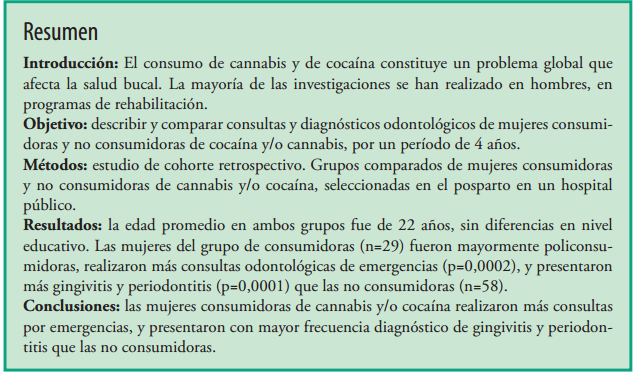
Abstract
Introduction:The use of cannabis and cocaine is a global problem that affects oral health. Most of the research has been performed on men, in rehabilitation programs.
Objective:to describe and compare dental attendances and oral diagnoses of women cannabis and/or cocaine users and non users, during 4 years.
Methods:retrospective cohort study. Compared groups of women who use and do not use cannabis and/or cocaine, selected in the postpartum period in a public hospital.
Results:the average age in both groups was 22 years, without educational level differences. Women in the consumers group (n= 29) were mostly polyconsumers, made more urgency dental attendances (p= 0.0002), and presented more gingivitis and periodontitis (p= 0.0001) than non-users (n= 58).
Conclusions:women who used cannabis and/or cocaine made more attendances for oral urgencies, and had a more frequent diagnosis of gingivitis and periodontitis than non-users.
References
Degenhardt L, Hall W. Extent of illicit drug use and dependence, and their contribution to the global burden of disease. Lancet. 2012;379(9810):55–70.
Teoh L, Moses G, McCullough MJ. Oral manifestations of illicit drug use. Aust Dent J. 2019;64(3):213-222.
Secretaria de políticas Integrales sobre Drogas de la Nación Argentina (SEDRONAR). Estudio nacional en población de 12 a 65 años sobre consumo de sustancias psicoactivas. Argentina, 2017. [Fecha de acceso: 12 de abril de 2021]. Disponible en: https://www.argentina.gob.ar/sedronar/investigaciony-estadisticas
Gigena Pablo C, Bella Marcela I, Cornejo Lila S. Salud bucal y hábitos de consumo de sustancias psicoactivas en adolescentes y jóvenes drogodependientes en recuperación. Odontoestomatología [Internet]. 2012; 14( 20 ): 49-59. [Fecha de acceso: 17 de abril de 2021]. Disponible en: http://www.scielo.edu.uy/scielo.php?script=sci_arttext&pid=S1688-93392012000200006&lng=es.
Antoniazzi RP, Zanatta FB, Rösing CK, Feldens CA. Association Among Periodontitis and the Use of Crack Cocaine and Other Illicit Drugs. J Periodontol. 2016;87(12):1396-1405.
Cury PR, Oliveira MG, Dos Santos JN. Periodontal status in crack and cocaine addicted men: a crosssectional study. Environ Sci Pollut Res Int. 2017 Feb;24(4):3423-3429.
Villarreal, M, Belmonte, V, Olivares, JL, & Abdala, A (2020). Trayectorias sanitarias de mujeres consumidoras de cocaína y/o cannabis durante el embarazo. Estudio de cohorte retrospectivo en La Pampa, Argentina. Revista De La Facultad De Ciencias Médicas De Córdoba; 77(2), 79-85. [Fecha de acceso: 7 de abril de 2021]. Disponible en: https://revistas.unc.edu.ar/index.php/med/article/view/26838
Thomson WM, Poulton R, Broadbent JM, et al. Cannabis smoking and periodontal disease among young adults. JAMA. 2008;299(5):525-531.
Keboa MT, Enriquez N, Martel M, Nicolau B, Macdonald ME. Oral Health Implications of Cannabis Smoking: A Rapid Evidence Review. J Can Dent Assoc. 2020 Jan;86:k2.
Mederos, M., Francia, A., Chisini, L. A., Grazioli, G., & Andrade, E. Influencia del consumo de cannabis en la enfermedad periodontal. Odontoestomatología 2018; 20(31). [Fecha de acceso: 7 de abril de 2021]. Disponible en http://www.scielo.edu.uy/scielo.php?script=sci_arttext&pid=S1688-93392018000100004
Chisini LA, Cademartori MG, Francia A, Mederos M, Grazioli G, Conde MCM, Correa MB. Is the use of Cannabis associated with periodontitis? A systematic review and meta-analysis. J Periodontal Res. 2019 Aug;54(4):311-317.
Chaparro-González NT, Fox-Delgado MA, Pineda- Chaparro RT, Perozo-Ferrer BI, Díaz-Amell AR, Torres V. Oral and maxillofacial manifestations in patients with drug addiction. Odontoestomatología 2018; 20(32):24-31. [Fecha de acceso: 7 de abril de 2021]. Disponible en: http://www.scielo.edu.uy/
scielo.php?script=sci_arttext&pid=S1688-93392018000200024&lng=es
Fernández-Martínez, N, Denis-Rodríguez, PB, Capetillo-Hernández, G. (2017) Periodontopatias y lesiones orales en consumidores de cocaína con ingreso reciente a un programa de rehabilitación en relación con pacientes no consumidores. Rev Mex Med Forense 2017, 2(1):19-26 . [Fecha de acceso: 15 de abril de 2021]. Disponible en: https://www.medigraphic.com/pdfs/forense/mmf-2017/mmf171c.pdf
Cury PR, Araujo NS, das Graças Alonso Oliveira M, Dos Santos JN. Association between oral mucosal lesions and crack and cocaine addiction in men: a cross-sectional study. Environ Sci Pollut Res Int. 2018 Jul;25(20):19801-19807.
Di Rienzo J.A., Casanoves F., Balzarini M.G., Gonzalez L., Tablada M., Robledo C.W. InfoStat versión 2019. Centro de Transferencia InfoStat, FCA, Universidad Nacional de Córdoba, Argentina. [Fecha de acceso: 12 de junio de 2021]. Disponible en: http://www.infostat.com.ar
Hakeberg, M., Wide Boman, U. Self-reported oral and general health in relation to socioeconomic position. BMC Public Health 18, 63 (2018). [Fecha de acceso: 21 de abril de 2021]. Disponible en: https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-017-4609-9#citeas
Paksoy T, Ustaoğlu G, Peker K. Association of socio-demographic, behavioral, and comorbidity-related factors with severity of periodontitis in Turkish patients. Aging Male. 2020;1:1-10.
Borrell LN, Beck JD, Heiss G. Socioeconomic disadvantage and periodontal disease: the Dental Atherosclerosis Risk in Communities Study. Am J Public Health. 2006;96(2):332–339. [Fecha de acceso: 22 de abril de 2021]. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1470476/
Baskaradoss JK, Geevarghese A. Utilization of dental services among low and middle income pregnant, post-partum and six-month post-partum women. BMC Oral Health. 2020 Apr 20;20(1):120. [Fecha de acceso: 10 de abril de 2021]. Disponible en: https://bmcoralhealth.biomedcentral.com/articles/10.1186/s12903-020-01076-9
Magri R, Míguez H, Parodi V, “et al”. Consumo de alcohol y otras drogas en embarazadas. Arch. Pediatr. Urug. 2007;78( 2 ):122-132. [Fecha de acceso: 22 de junio de 2021]. Disponible en http://www.scielo.edu.uy/scielo.php?script=sci_arttext&pid=S1688-12492007000200006
Versteeg PA, Slot DE, van der Velden U, van der Weijden GA. Effect of cannabis usage on the oral environment: a review. Int J Dent Hyg. 2008;6 (4): 315–20.
Ramo DE, Delucchi KL, Hall SM, Liu H, Prochaska JJ. Marijuana and tobacco co-use in young adults: patterns and thoughts about use. J. Stud. Alcohol Drugs. 2013;74:301–310. [Fecha de acceso: 7 de abril de 2021]. Disponible en https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3568169/
Yazdanian M, Armoon B, Noroozi A, Mohammadi R, Bayat AH, Ahounbar E, Higgs P, Nasab HS, Bayani A, Hemmat M. Dental caries and periodontal disease among people who use drugs: a systematic review and meta-analysis. BMC Oral Health. 2020 Feb 10;20(1):44. [Fecha de acceso: 10 de abril de 2021]. Disponible en: https://pubmed.ncbi.nlm.nih.gov/32041585/
Hartnett E, Haber J, Krainovich-Miller B, Bella A, Vasilyeva A, Lange Kessler J. Oral Health in Pregnancy. J Obstet Gynecol Neonatal Nurs. 2016 Jul Aug;45(4):565-73.
Güncü GN, Tözüm TF, Çaglayan F. Effects of endogenous sex hormones on the periodontium - review of literature. Aust Dent J. 2005;50(3):138–145.
Brondani MA, Alan R, Donnelly L. Stigma of addiction and mental illness in healthcare: The case of patients’ experiences in dental settings. PLoS One. 2017 May 22;12(5):e0177388. . [Fecha de acceso: 18 de abril de 2021]. Disponible en: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0177388
Ilgen M, Edwards P, Kleinberg F, Bohnert AS, Barry K, Blow FC. The prevalence of substance use among patients at a dental school clinic in Michigan. J Am Dent Assoc. 2012 Aug;143(8):890-6.
Schatman ME, Patterson E, Shapiro H. Patient Interviewing Strategies to Recognize Substance Use, Misuse, and Abuse in the Dental Setting. Dent Clin North Am. 2020 Jul;64(3):503-512.
Fischer RG, Lira Junior R, Retamal-Valdes B, Figueiredo LC, Malheiros Z, Stewart B, Feres M. Periodontal disease and its impact on general health in Latin America. Section V: Treatment of periodonti tis. Braz Oral Res. 2020 Apr 9;34(supp1 1):e026. [Fecha de acceso: 20 de abril de 2021]. Disponible
en https://www.scielo.br/scielo.php?script=sci_arttext&pid=S1806-3242020000200604
Marouf N, Cai W, Said KN, Daas H, Diab H, Chinta VR, Hssain AA, Nicolau B, Sanz M, Tamimi F. Association between periodontitis and severity of COVID-19 infection: A case-control study. J Clin Periodontol. 2021;48:483-491.

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.