Resumen
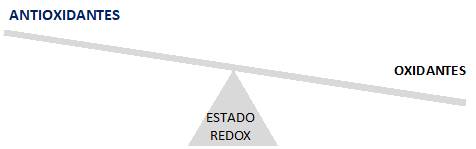
Resumen: Numerosos reportes demuestran la presencia de biomarcadores de estrés oxidativo en la saliva de fumadores y hay un creciente interés en correlacionar estos procesos moleculares con la etiología de algunas enfermedades orales, como la periodontitis, una enfermedad inmunoinflamatoria crónica relacionada con un desequilibrio de la homeostasis redox celular.
Objetivo: realizar una revisión narrativa sobre la relación entre la disminución de la capacidad antioxidante salival inducida por humo de tabaco, la periodontitis y el potencial uso de farmacología redox para el tratamiento de esta patología.
Métodos: se realizó una búsqueda bibliográfica en bases de datos como PUBMED (NLM, NIH, NCBI) y SciELO.
Resultados: existe evidencia que relaciona la baja capacidad antioxidante salival con un retraso en el restablecimiento de las condiciones normales en la cavidad oral ante el desarrollo de periodontitis. A su vez, el estado inflamatorio asociado colabora sinérgicamente, provocando un mayor daño tisular con pérdida de tejidos de soporte dentario, fenómeno que podría ser modulado por la acción de farmacología redox.
Conclusiones: la intervención con farmacología redox, podría atenuar los biomarcadores de progresión de la enfermedad periodontal, constituyendo una herramienta prometedora para utilizar en conjunto con las estrategias de tratamiento tradicionales.
Referencias
2. Edgar M, Dawes C, O’Mullane D. Saliva and Oral Health [Internet]. 4ta ed. Stephen Hancocks Limited; 2012. Available from: https://wrigleyoralhealth.com/content/docs/SHL_S_OH_A5_2015_FINAL.pdf
3. Knaś M, Maciejczyk, D, Zalewska A. Oxidative stress and salivary antioxidants. Dent Med Probl. 2013;50(4):5.
4. Żukowski P, Maciejczyk M, Waszkiel D. Sources of free radicals and oxidative stress in the oral cavity. Arch Oral Biol [Internet]. 2018;92:8–17. Available from: https://doi.org/10.1016/j.archoralbio.2018.04.018
5. Huang Chang C, Lun Han M, Teng NC, Yu Lee C, Ting Huang W, Tong Lin C, Kai Huang Y. Cigarette Smoking Aggravates the Activity of Periodontal Disease by Disrupting Redox Homeostasis- An Observational Study. Sci Rep. 2018;8(11055).
6. Toczewska J; Konopka T, Zalewska A, Maciejczyk M. Nitrosative Stress Biomarkers in the Non Stimulated and Stimulated Saliva, as well as Gingival Crevicular Fluid of Patients with Periodontitis: Review. Antioxidants (Basel, Switzerland). 2020;9(3):14.
7. Dahiya P, Kamal R, Gupta R, Bhardwaj R, Chaudhary K, Kaur S. Reactive oxygen species in periodontitis. J Indian Soc Periodontol. 2013;17(4):411–6.
8. Sies H. Oxidative Stress: Introductory Remarks, in Oxidative Stress. 1era ed. Sies H, editor. Academic Press; 1985. 1–8 p.
9. Sies H, Berndt C, Jones D. Oxidative stress. Annu Rev Biochem. 2017:715–48.
10. Radi R. Evolución del concepto de “Estrés Oxidativo”: medio siglo de aportes de la Facultad de Medicina, Montevideo, Uruguay. Anales de Facultad de Medicina [Internet]. 2014: 9–22. Available from: https://revistas.udelar.edu.uy/OJS/index.php/anfamed/article/view/225/216
11. Iannitti T Rottigni V, Palmieri B. Role of free radicals and antioxidant defences in oral cavity-related pathologies. J Oral Pathol Med. 2012;41(9):649–61.
12. Sies H. Oxidative eustress: On constant alert for redox homeostasis. Redox Biol. 2021;41(101867):8.
13. Sies H, Jones D. Reactive oxygen species (ROS) as pleiotropic physiological signalling agents. Nat Rev Mol Cell Biol. 2020;21(7):363–83.
14. Radi R. Oxygen radicals, nitric oxide, and peroxynitrite: Redox pathways in molecular medicine. Proc Natl Acad Sci U S A . 2018;115(23):5839–48.
15. Halliwell B. Reactive Species and Antioxidants. Redox Biology Is a Fundamental Theme of Aerobic Life. Am Soc Plant Biol. 2006;141:312–22.
16. Battino M, Ferreiro MS, Gallardo I, Newman HN, Bullon P. The antioxidant capacity of saliva. J Clin Periodontol [Internet]. 2002 Mar;29(3):189–94. Available from: http://doi.wiley.com/10.1034/j.1600-051X.2002.290301x.x
17. Valez V. Producción de radicales libres en sistemas biológicos y su detección mediante quimioluminiscencia [Tesis de grado]. [Montevideo]: Universidad de la República; 2006.
18. D’Autréaux B, Toledano MB. ROS as signalling molecules: mechanisms that generate specificity in ROS homeostasis. Nat Rev Mol cell Biol. 2008;8:813–824.
19. Augusto O, Miyamoto S. Radicals and related species. In: Pantopoulus, K; Schipper H, editor. Principles of free radical biomedicine. New York: Nova biomedical; 2012.
20. Poderoso JJ. El Premio Nobel 1998: la resurrección de un gas inorgánico como una molécula de alta significación biológica. Dep Med y Lab Metab Oxígeno Hosp Clínicas José San Martín Fac Med UBA [Internet]. 199AD;205–7. Available from: http://www.medicinabuenosaires.com/revistas/vol59-99/2/v59_n2_205_207.pdf
21. Ignarro LJ. Biosynthesis and Metabolism of Endothelium-Derived Nitric Oxide. Annu Rev. 1990;50:535–60.
22. Denicola A, Souza J, Radi R. Diffusion of peroxynitrite across erythrocyte membranes. Proc Natl Acad Sci USA. 1998;95:3566–357.
23. Radi R, Peluffo G, Alvarez MN, Naviliat M, Cayota A.Unraveling peroxynitrite formation in biological systems. Free Radic Biol Med. 2001;30(5):463–88.
24. Trujillo M, Ferrer-Sueta G, Radi R. Peroxynitrite detoxification and its biologic implications. Antioxid Redox Signal. 2008;9:1607–20.
25. Waszkiewicz N, Bejda G, Zalewska A, Maciejczyk M. Diagnostic Value of Salivary Markers in Neuropsychiatric Disorders. Dis Markers [Internet]. 2019;6. Available from: https://doi.org/10.1155/2019/4360612
26. Akalin FA, Baltacioglu E, Alver A, Karabulut E. Lipid peroxidation levels and total oxidant status in serum, saliva and gingival crevicular fluid in patients with chronic periodontitis. J Clin Periodontol. 2007;34:558–65.
27. Halliwell B, Gutteridge JMC. Free radicals in biology and medicine. 4ta ed. New York: Oxford University Press Inc.; 2010. 79–178 p.
28. Fridovich I. Superoxide dismutases. An adaptation to a paramagnetic gas. J Biol Chem. 1989;264(14):7761–4.
29. Narendra S, Das UK, Tripathy SK, Sahani NC. Superoxide Dismutase, Uric Acid, Total Antioxidant Status, and Lipid Peroxidation Assay in Chronic and Aggressive Periodontitis Patients. J Contemp Dent Pr. 2018;19(7):874–80.
30. Sardaro N, Della Vella F, Incalza MG, Di Stasio D, Lucchese A, Contaldo M, Laudadio C, Petruzzi M. Oxidative Stress and Oral Mucosal Diseases: An Overview. In Vivo (Brooklyn). 2019;33(2):289–96.
31. Permuy M, López-Peña M, González-Cantalapiedra A, Muñoz F. Melatonin: A Review of Its Potential Functions and Effects on Dental Diseases. Int J Mol Sci. 2017;18(865):13.
32. Meenakshi S, Malaiappan S. Role of melatonin in periodontal disease - A systematic review. Indian J Dent Res. 2020;31(4):593–600.
33. Ghallab N, Hamdy E, Shaker O. Malondialdehyde, superoxide dismutase and melatonin levels in GCF of aggressive and chronic periodontitis patients. Aust Dent J. 2016;61(1):53–61.
34. Neslihan Avan A, Demirci Çekiç S, Uzunboy C, Apak R. Spectrophotometric Determination of Phenolic Antioxidants in the Presence of Thiols and Proteins. Int J Mol Sci. 2016;17(1325):16.
35. do Valle I, Roweth H , Malloy M, Moco S, Barron D, Battinelli E, Loscalzo J Barabási A-L. Network Medicine Framework Shows Proximity of Polyphenol Targets and Disease Proteins is Predictive of the Therapeutic Effects of Polyphenols. BioRxiv. 2021;35.
36. Javed F, Rahman I, Romanos G. Tobacco-product usage as a risk factor for dental implants. Periodontol 2000. 2019;81(1):48–56.
37. Gutierrez Maydata A. Oxidantes en el humo del cigarro y enfermedades cardiopulmonares. Rev Cuba med [Internet]. 2003;42(5). Available from: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S0034-75232003000500009&lng=es
38. van der Velden U, Abbas F Armand, S Loos BG, Timmerman MF, Van der Weijden GA, Van Winkelhoff AJ ,Winkel EG. Java project on periodontal diseases. The natural development of periodontitis: risk factors, risk predictors and risk determinants. J Clin Periodonto. 2006;33(8):540–8.
39. Ali Mosaddad S, Tahmasebi E, Yazdanian A, Bagher Rezvani M, Seifalian A, Yazdanian M, Tebyanian H. Oral microbial biofilms: an update. Eur J Clin Microbiol Infect Dis. 2019;38(11):2005–19.
40. De Luca F, Shoenfeld Y. The microbiome in autoimmune diseases. Clin Exp Immunol. 2019;195(1):74–85.
41. Landzberg, M, Doering H, Aboodi GM, Tenenbaum, HC, Glogauer M. Quantifying oral inflammatory load: oral neutrophil counts in periodontal health and disease. Periodontal Res. 2015;50(3):330–6.
42. Chapple IL, Brock GR, Milward MR, Ling N, Matthews JB. Compromised GCF total antioxidant capacity in periodontitis: cause or effect? J Clin Periodonto. 2017;34(2):103–10.
43. Buczko P, Zalewska A, Szarmach I. Saliva and oxidative stress in oral cavity and in some systemic disorders. J Physiol Pharmacol. 2015;66(1):3–9.
44. Toczewska J, Maciejczyk M, Konopka TZA. Total Oxidant and Antioxidant Capacity of Gingival Crevicular Fluid and Saliva in Patients with Periodontitis: Review and Clinical Study. MDPI - Publ Open Access Journals. 2020;9(450):16.
45. Tóthová, L, Kamodyová N, Červenka T, Celec P. Salivary markers of oxidative stress in oral diseases. Front Cell Infect Microbiol. 2015;5(73).
46. Poprack P, Jomova K, Simunkova M, Kollar V, Rhodes C, Valko M. Targeting free radicals in oxidative stress- related human diseases. Trends Pharmacol Sci. 2017;38(7):592–607.
47. Ambati M, Rekha Ran K, Veerendranath Reddy P, Suryaprasanna J, Dasari R, Gireddy H. Evaluation of oxidative stress in chronic periodontitis patients following systemic antioxidant supplementation: A clinical and biochemical study. J Nat Sci Biol Med. 2017;8(1):99–103.
48. Sczepanik FSC, Grossi ML, Casati M ,Goldberg M, Glogauer M, Fine N, Tenenbaum HC. Periodontitis is an inflammatory disease of oxidative stress: We should treat it that way. Periodontol 2000. 2020;54(1):45–68.
49. Sui L, Wang J, Xiao Z, Yang Y, Yang Z, Ai K. ROS-Scavenging Nanomaterials to Treat Periodontitis. Front Chem. 2020;8(595530):6.
50. Toker H, Ozdemir H, Balcı H, Ozer H. N-acetylcysteine decreases alveolar bone loss on experimental periodontitis in streptozotocin-induced diabetic rats. J Periodontal Res. 2012;47(6):793–9.