Abstract
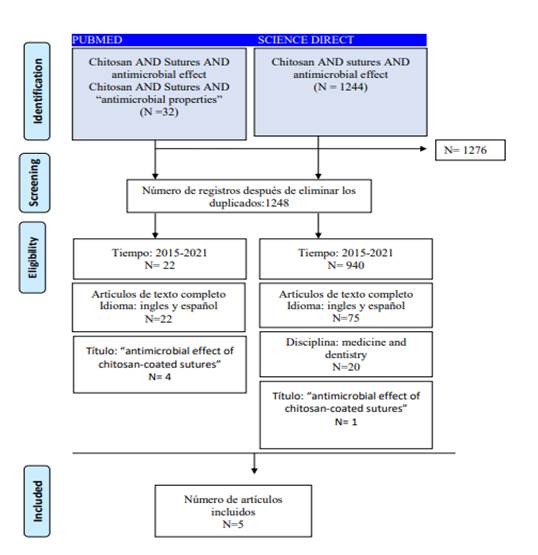
Postoperative infections are increasingly common, as well as the resistance of these causative bacteria to antibiotics, which is why the need to look for a natural material with biocompatibility and antimicrobial properties used in the coating of sutures, since these are considered an intrinsic factor in the process of these complications. The objective of this review is to carry out a systematic search on the antimicrobial effectiveness of chitosan used in the coating of sutures in oral and maxillofacial surgery. The search was carried out in two databases: PubMed and ScienceDirect from February to March 2021. PRISMA guidelines for systematic reviews were followed. The five included articles from in vitro or in vivo studies showed that chitosan coating of sutures inhibits Gram (+) and Gram (-) microorganisms, exhibiting greater activity against Gram (-). It is concluded that the coating of sutures with chitosan could supplement and improve the properties of currently commercial antimicrobial sutures, reduce postoperative infections, and accelerate the healing processes.
References
2. Frank LA, Onzi GR, Morawski AS, Pohlmann AR, Guterres SS, Contri RV. Chitosan as a coating material for nanoparticles intended for biomedical applications. Reactive and Functional Polymers. 2020; (147):104459.
3. Cicciú M, Fiorillo L, Cervino G. Chitosan use in dentistry: systematic review of recent clinical studies. Mar Drugs 2019;17(7):417.
4. Chenxi Z, Didi H, Colin D, Huan S, Wei P, Xiaobing P, Zhengyong L, Jianxun S, Changchun Z. Preparation and application of chitosan biomaterials in dentistry. Review. Int J Biol Macromol 2021;15(167):1198-1210.
5. Poblete F, Dallaserra M, Yanine N, Araya I, Cortés R, Vergara C, Villanueva J. Incidencia de complicaciones posquirúrgicas en cirugía oral. Int J Interdiscip Dent 2020; 13(1):13-16.
6. Despaigne I, Rodríguez Z, Pascual M, Lozada GA, Mustelier HL. Consideraciones actuales sobre las infecciones posoperatorias. Review. MEDISAN. 2013;17(4): 686-707.
7. Lestari W, Yusry WN, Haris MS, Jaswir I, Idrus E. A glimpse on the function of chitosan as a dental hemostatic agent. Japan Dental Science Review 2020;56(1):147-154.
8. Viju S, Thilagavathi G. Effect of chitosan coating on the characteristics of silk-brained sutures. Journal of Industrial Textiles 2012;42(3):256-268.
9. Minozzi F, Bollero P, Unfer V, Dolci A, Galli M. The sutures in dentistry.Eur Rev Med Pharmacol Sci 2009;13(3):217-26.
10. Shlomo M, Avital K, Anda KS, Levartovskya Y, Mazora H. The effect of commonly used sutures on inflammation inducing pathogens – An in vitro study. J Craniomaxillofac Surg 2013;41(7):593-7.
11. Xiaojie C, Dandan H, Xiaoqi T, Lu W. Quantitative physical and handling characteristics of novel antibacterial braided silk suture materials. J Mech Behav Biomed Mater 2015;(50):160-70.
12. Ayala G. Efecto antimicrobiano del quitosano: una revisión de la literatura. Scientia Agroalimentaria. 2015;(2):32-38.
13. Clayton EM, Todd M, Dowd JB, Aiello AE. The impact of bisphenol A and triclosan on immune parameters in the U.S. population, NHANES 2003-2006. Environ Health Perspect. 2011;119(3):390-6.
14. Serrano C, García L, Fernández JP, Barbeck M, Ghanaati S, Unger R, Kirkpatrick J, Arzt E, Funk L, Turon P, del Campo A. Nanoestructured medical sutures with antibacterial properties. J Biomaterials. 2015;(52):291-300.
15. Hutton B, Ferrán C, López F., Moher D. La extensión de la declaración PRISMA para revisiones sistemáticas que incorporan metaanálisis en red: PRISMA-NMA. Medicina. 2016;(16):262-266.
16. Masood R, Hussain T, Umar M, Azeemullah, Areeb T, Riaz S. In situ development and application of natural coatings on non-absorbable sutures to reduce incision site infections. J Wound Care. 2017;26(3):115-120.
17. Prabha S, Sowndarya J, Ram PJVS, Rubini D, Hari BNV, Aruni W, Nithyanand P. Chitosan-Coated Surgical Sutures Prevent Adherence and Biofilms of Mixed Microbial Communities. Curr Microbiol 21;78(2):502-512.
18. Debbabi F, Gargoubi S, Hadj Ayed MA, Abdessalem SB. Development and characterization of antibacterial braided polyamide suture coated with chitosan-citric acid biopolymer. J Biomater Appl 2017;32(3):384-398.
19. Mohammadi H, Alihosseini F, Hosseini SA. Improvement of the physical and biological properties of monofilament nylon as chitosan/hyaluronic acid suture. Int J Biol Macromol 2020; 164:3394-3402.
20. Yang Y, Yang SB, Wang YG, Zhang SH, Yu ZF, Tang TT. Bacterial inhibition potential of quaternised chitosan-coated
VICRYL absorbable suture: An in vitro and in vivo study. Journal of orthopaedic translation. 2016;11(8):49-61.
21.Kong M, Chen XG, Xing K, Park HJ. Antimicrobial properties of chitosan and mode of action: A state of the art review.
International Journal of Food Microbiology. 2010;144(1):51-63.
22. Yuanhong L, Ya-Qui C, Chen- Hao Y, Yu X, Meng.Ying X, Chao-Liang Z, Xianglong H, Qiang P. Drug-free and non-cross-linked chitosan scaffolds with effective antibacterial activity against Gram-negative and Gram-positive bacteria. Carbohydrate Polymers. 2020;(241):116386.
23. H. Bellanger, Casdorff K, F. Muff L, Ammann R, Burgert I, Michen B. Layer-by-layer deposition on heterogeneous surface: Effect of sorption kinetics on the growth of polyelectrolyte multilayers. Journal of Colloid and Interface Science.2017;(500):133-141.